The human body is nothing short of a well-designed machine. Each of our organs has a specific role to play- which is why they hold unique positions within our body. However, if an internal organ shifts and moves into an unfamiliar position, it causes conditions like organ prolapse or hernia.
Rectal prolapse is one such condition when the rectum- which is the lower end of the large intestine- falls out of its normal position in the pelvic region. Studies show that about 2.5 people out of 100,000 are affected by this condition. It is relatively rare; however, women over the age of 50 have a risk six times higher to have this condition. Rectal prolapse is also common among older adults with a long-term history of pelvic floor weakness or constipation. It is also found among infants and older children.
In this blog, we will discuss this condition more in detail and when you should consult with a proctologist.
Rectal prolapse: What is it all about?
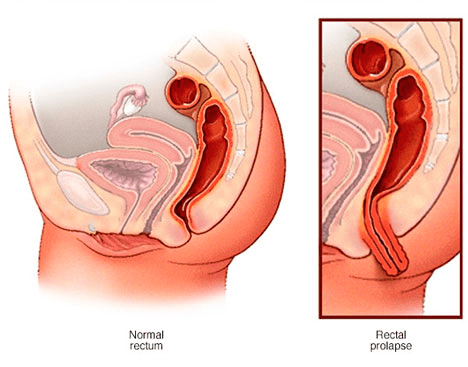
Rectal prolapse is a condition when the rectum falls from its normal position in the pelvic area and protrudes through the anus. Typically, there are 3 types of rectal prolapse-
- Full-thickness: This is the most common type of rectal prolapse. Here, the full thickness of the wall of the rectum falls through the anus.
- Mucosal: This is a type of prolapse where the lining of the anus or mucosa sticks out through the anus.
- Internal: An internal prolapse occurs when the rectum folds on itself, bud does not come out of the anus.
Due to its nature, rectal prolapse is often confused with haemorrhoids. In some cases, early-stage rectal prolapse may look like internal haemorrhoids that are pushed out of the anus, making it difficult for physicians to differentiate between both. In some cases, haemorrhoids are associated with mucosal rectal prolapse. However, these two conditions are very different. While rectal prolapse occurs due to the slippage of the rectum into the anus, haemorrhoids are swollen blood vessels that develop in the anus and lower rectum. Haemorrhoids are often accompanied by anal itching, discomfort, pain and bleeding during and after bowel movements. The symptoms of a rectal prolapse appear differently and must be mentioned to your proctologist during the consultation to get a proper diagnosis.
Rectal prolapse: Symptoms and causes
If you have a rectal prolapse, you may feel a bulge, along with the appearance of a reddish-coloured mass sticking out of your anus. More often than not, the first occurrence is during or after a bowel movement. But over time, even simple everyday movements like walking or standing may cause the end of the rectum to come out of the anal canal, requiring you or a medical professional to push it back up into the anus manually.
People suffering from rectal prolapse may also suffer from faecal incontinence with leakage of mucus, stool or blood from the anus. This is due to the prolapsing bowel keeping the anal canal open and the continuous stretching of the anal muscles that can ultimately affect their function. Rectal prolapse may be accompanied by pain in the anus and bleeding from the inner lining of the rectum. Although the symptoms are not life-threatening, they should be taken seriously.
If you suffer from symptoms and suspect a rectal prolapse, don’t shy away from visiting a proctology doctor. Sometimes the prolapsed tissue can become strangulated, which cuts off circulation in the tissues. This causes the tissue to become necrotic and die. To avoid such situations, you must treat this condition as a serious medical emergency and consult with a proctologist at the earliest.
Rectal prolapse: How does it happen?
What exactly causes the rectum to slide down from its position and eventually prolapse? Studies show that an estimated 30% to 67% of patients with rectal prolapse have chronic constipation and 15% suffer from frequent diarrhoea. Earlier, doctors linked this condition to vaginal birth. However, today we know that 35% of patients with rectal prolapse never gave birth. So far we know that rectal prolapse can occur as a result of many conditions that people generally do not pay attention to. These include-
- A long history of straining during bowel movement
- Chronic diarrhoea or constipation
- Injuries to the anal or pelvic region
- Nerve damage due to pregnancy, difficult vaginal childbirth, anal sphincter paralysis, spinal injury, back injury, back surgery or any other surgeries in the pelvic area
- Weakness of anal sphincters following direct injury or nerve damage
- Weakness of the ligaments and support system of the rectum due to old age
- Other conditions, e.g. infections and diseases including cystic fibrosis, chronic obstructive pulmonary disease, diabetes, hysterectomy, intestinal infections caused by parasites, and digestive issues caused by poor nutrition
Diagnosing rectal prolapse
The sooner you consult with your proctologist in Dubai, the faster you will receive your diagnosis and treatment. During the consultation, your doctor will ask for your medical history and perform a rectal exam. You may be asked to mimic an actual bowel movement by straining while sitting on a commode. This will help to show the prolapse, and the doctor can confirm the diagnosis and move forward with a treatment plan.
To make a sound diagnosis, your proctology doctor may rely on several tests. These tests help in evaluating your condition and help the doctor make the best treatment decision. Some of these tests are-
- Anal electromyography is used to determine nerve damage. This test is recommended to identify the reason for the improper functioning of the anal sphincters or pelvic floor muscles.
- Anal manometry is used to study the strength and tone of the anal sphincter muscles by inserting a small thin tube up into the anus and rectum.
- Anal ultrasound is used to evaluate the shape and structure of the anal sphincter muscles and surrounding tissue. Here, the images of the sphincters are taken by inserting a small probe into the anus and rectum.
- Proctography is a radiology test where an x-ray video of the rectum during bowel movement is recorded. It helps the doctor understand the capacity of the rectum, abnormal movements, changes in its position, and how well it can hold the stool and release them during a bowel movement.
- Colonoscopy is an examination of the colon or large intestine. A flexible tube fitted with a camera is passed through the anus towards the point where the large intestine joins the small intestine. This helps to identify underlying issues related to the prolapse and rule out other conditions.
- Proctosigmoidoscopy is a test that allows you to observe the lining of the lower portion of the colon. A flexible tube with an attached camera is inserted into the rectum up to the sigmoid colon to look for inflammation, ulcers, polyp or tumour.
- MRI or Magnetic resonance imaging is a radiology test used to evaluate various parts of the body, including pelvic organs. This is usually combined with a proctogram to obtain dynamic information.
Your proctologist may recommend any of these tests to observe and study your issue further. Sometimes, weak pelvic floor and structures will cause other conditions like urinary incontinence, bladder prolapse and vagina/uterine prolapse alongside rectal prolapse. As these issues require an expert opinion from other specialists like urologists and gynaecologists, your proctologist may work with them as a team to share evaluations and make joint treatment decisions.
Treatment and management of rectal prolapse
Minor cases of prolapse are often treated at home with the help of stool softeners and by pushing the prolapsed tissue back into the anus when required. In case the issue is recurrent, your proctologist will suggest a surgical repair.
There are several surgical approaches to correct the prolapse. Doctors discuss different options with the patients after taking into consideration their age, health conditions and extent of the prolapse. Abdominal and perineal (through the anus) surgeries are the two surgical approaches used to repair rectal prolapse.
The abdominal procedure is recommended for individuals who are healthy and don’t present any other health issues. The procedure is done under general anaesthetic and usually using minimally invasive surgery (laparoscopy or robotic surgery). There are two types of repair-
- Rectopexy: Reattachment of the rectum using sutures or meshes. This is often done as a laparoscopic or robotic procedure, ensuring faster recovery.
- Resection Rectopexy: Removal of a section of the large intestine ( Sigmoid colon) followed by rectopexy. This is recommended for patients with severe constipation.
The rectal or perineal repair was in the past more commonly recommended for older patients and individuals with other medical conditions. However, modifications of techniques and the introduction of new stapling devices have allowed widespread use of this approach. A perineal or rectal repair can be performed under general or spinal anaesthesia.
There are three most common rectal approaches-
- Altemeier procedure: The part of the rectum coming out of the anus is cut off and the ends are sewn together. Additionally, the muscular structures of the pelvic floor are stitched back together for better support.
- Delorme procedure: Here the inner lining of the prolapsed rectum is removed. The muscle layer is bunched up with sutures and the inner lining is finally sutured back. The rectum is pushed back into the anus.
- Stapled Resection of Rectum (STARR): In this procedure, a stapling gun is introduced into the anus and the prolapse is removed with the edges stapled together at the same time.
These surgical interventions resolve the problem with the prolapse and improve the quality of life. However, as with any surgery, these procedures come with certain risks including anaesthesia complications, bleeding, infection. In some cases, the ends of the bowel that were reconnected after a surgery fail to heal properly leading to leakage.
The prolapse may also return in some patients, worsening or developing faecal incontinence/constipation. Patients recovering from prolapse surgery are advised to consume fibrous foods, drink plenty of fluids and also take stool softeners or mild laxatives to avoid constipation and straining.
Generally, the outlook of rectal prolapse surgery is dependent on the age and health of the patient. The results can also vary depending on the condition of the supporting tissues in the pelvic region. While all the procedures discussed above solve the prolapse, abdominal procedures generally tend to have better results when compared to perineal procedures.
The use of minimally invasive techniques(laparoscopic or robotic) for the abdominal treatment of prolapse allows for a short stay in the hospital and a quick return to everyday activities. Recovery from perineal procedures is usually quicker and patients can be discharged on the same day.
Takeaway
Rectal prolapse is not very common, but it can be a very debilitating condition. While there are several factors linked to rectal prolapse, there is no clear cut answer as to what causes it. As the symptoms of rectal prolapse overlap with other conditions, diagnosis gets sometimes delayed. Therefore, if you experience any of the symptoms we have discussed in this blog, it is best to consult with one of the best proctologists in Dubai, Dr Antonio Privitera. Book your appointment for a comprehensive consultation with this renowned surgeon today.