Hemorrhoids (Piles) Treatment in Dubai
Here’s what sets our approach apart:
- Accurate diagnosis first: We examine you properly (visual inspection, digital exam, anoscopy when needed) to confirm hemorrhoids and rule out other causes of your symptoms—including fissures, fistulas, polyps, or colorectal cancer.
- Grade-based treatment: A Grade 1 internal hemorrhoid responds well to dietary changes; a Grade 4 prolapsed hemorrhoid usually needs surgery. We match the treatment to your condition, not the other way around.
- Discreet, same-day assessment available: Privacy matters. We offer consultations at multiple locations across Dubai and Abu Dhabi, with flexible scheduling and complete confidentiality.
This guide explains everything you need to know about hemorrhoids, from symptoms and diagnosis to the full range of treatment options available in the UAE.
Table of Contents
- 1. What Are Hemorrhoids?
- 2. It's Not Always Hemorrhoids: What Else Could It Be?
- 3. Red Flags: When You Need Urgent Evaluation
- 4. Internal vs External Hemorrhoids: Why the Difference Matters
- 5. Hemorrhoid Grading System: Why It Changes Everything
- 6. What Causes Hemorrhoids? (And Dubai-Specific Risk Factors)
- 7. Treatment Options in Dubai: From Conservative Care to Surgery
- 8. Recovery: What to Expect After Treatment
- 9. My Approach: What Sets This Practice Apart
- 10. Frequently Asked Questions
- 11. References and Medical Sources
- 12. Locations and Booking
What Are Hemorrhoids?
Hemorrhoids (also called piles) are swollen blood vessels in the lower rectum and anal canal. Everyone has hemorrhoidal tissue—these vascular cushions help with continence and sensation. Hemorrhoids become a problem when they enlarge, bleed, prolapse (come out of the anus), or cause pain.
There are two types:
Internal hemorrhoids: Sit inside the rectum, above the dentate line (the boundary between rectal tissue and anal skin). You usually can't see or feel them. They're covered by rectal mucosa, which has no pain receptors, so internal hemorrhoids typically don't hurt—they bleed.
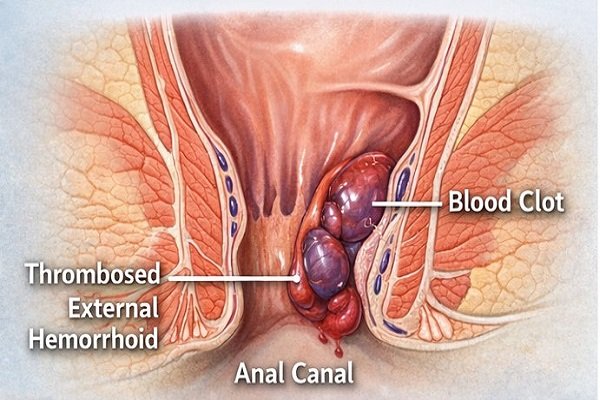
External hemorrhoids: Are under the skin around the anus, below the dentate line. Because this area has pain receptors, external hemorrhoids can be painful, especially if a clot forms inside them (thrombosed external hemorrhoid).
Hemorrhoids are extremely common, with many adults experiencing symptoms at some point in their lives, particularly between ages 45 and 65, though they can also appear in patients in their 20s and 30s, especially in sedentary populations.
Symptoms of Hemorrhoids: What You Might Notice
Hemorrhoid symptoms vary depending on whether they're internal or external, and what grade they are. Here's what patients typically experience:
Bleeding
Bright red blood on toilet paper, in the toilet bowl, or on the surface of stool. This is the most common symptom of internal hemorrhoids. The bleeding is usually painless and happens during or just after a bowel movement. If you see blood, it's important to get checked—while hemorrhoids are a common cause of rectal bleeding, other conditions (fissures, polyps, inflammatory bowel disease, cancer) can also cause bleeding.
A lump or swelling
You might feel a soft lump near your anus. This could be a prolapsed internal hemorrhoid (one that's come out through the anus) or an external hemorrhoid. If the lump appeared suddenly and is painful, it may be a thrombosed external hemorrhoid (a clot inside).
Itching or irritation
Mucus discharge from prolapsing internal hemorrhoids can irritate the anal skin, causing itching (pruritus ani). Moisture and poor cleaning can make this worse.
Discomfort or pain
Internal hemorrhoids usually don't hurt unless they prolapse and become strangulated (blood supply is cut off). External hemorrhoids can be uncomfortable, and thrombosed external hemorrhoids are often very painful for the first 48–72 hours.
Mucus discharge or soiling
When internal hemorrhoids prolapse, they can leak mucus, leading to a feeling of dampness and sometimes minor staining of underwear.
A feeling of incomplete evacuation
Large internal hemorrhoids can make you feel like you haven't fully emptied your bowels.
When symptoms mean something more serious:
If you experience heavy bleeding, severe pain with fever, sudden weakness or dizziness, significant weight loss, or a change in bowel habits (new constipation or diarrhea lasting more than a few weeks), you need urgent evaluation. These can be signs of other conditions that require immediate attention.
It's Not Always Hemorrhoids: What Else Could It Be?
This is one of the most important parts of my role as a colorectal surgeon: not assuming that rectal bleeding or anal discomfort is automatically hemorrhoids. I've seen too many patients who were told they had hemorrhoids based on symptoms alone, without proper examination.
Here are other conditions that can cause similar symptoms:
Anal fissure
A tear in the anal lining, usually caused by passing hard stool. Fissures cause sharp pain during and after bowel movements, and you may see a small amount of bright red blood. Unlike hemorrhoids, fissures hurt significantly.
Anal fistula
An abnormal tunnel between the inside of the anal canal and the skin near the anus, usually resulting from an infection (abscess). Fistulas cause discharge (pus, blood, or mucus), irritation, and sometimes pain. They don't resolve on their own and require treatment.
Anal abscess
A collection of pus near the anus, causing severe pain, swelling, fever, and difficulty sitting. This is a surgical emergency.
Polyps or colorectal cancer
Polyps (growths on the colon lining) and cancer can both cause rectal bleeding. The blood may be darker (maroon or mixed with stool) or bright red. This is why screening matters, especially after age 40 in the UAE.
Inflammatory bowel disease (IBD)
Conditions like Crohn's disease or ulcerative colitis cause bleeding, diarrhea, abdominal pain, and weight loss. These require very different treatment from hemorrhoids.
Rectal prolapse
The rectum itself protrudes through the anus (different from a prolapsed hemorrhoid). This usually requires surgical repair.
This is why examination matters. A proper assessment includes a visual inspection, a digital rectal exam, and often anoscopy (a small scope to look inside the anal canal). If there are any red flags—your age, family history, blood mixed with stool rather than separate, weight loss—I'll recommend colonoscopy to examine the entire colon.
Red Flags: When You Need Urgent Evaluation
Most hemorrhoid symptoms are not dangerous, but certain signs should prompt you to seek medical care quickly:
- Heavy bleeding that soaks through toilet paper or causes clots in the toilet
- Bleeding with dizziness, weakness, or fainting (possible anemia)
- Severe, constant pain (not just discomfort during bowel movements)
- Fever with anal pain or swelling (possible abscess)
- Significant, unexplained weight loss (more than 5 kg in a few months)
- Change in bowel habits lasting more than 2–3 weeks (new constipation, diarrhea, or narrowing of stool)
- Blood that's dark, maroon, or mixed throughout the stool (rather than bright red on the surface)
- Any rectal bleeding if you're over 40 and haven't been screened for colon cancer
In the UAE, colorectal cancer screening typically starts at age 40, earlier than in some other countries. This reflects both local population demographics and alignment with international guidelines from the Abu Dhabi Department of Health and Cleveland Clinic Abu Dhabi. If you're 40 or older and experiencing any rectal bleeding—even if you're certain it's hemorrhoids—it's important to undergo colon screening (usually colonoscopy) to rule out polyps or cancer. Early detection of colorectal cancer is highly treatable.
Internal vs External Hemorrhoids: Why the Difference Matters
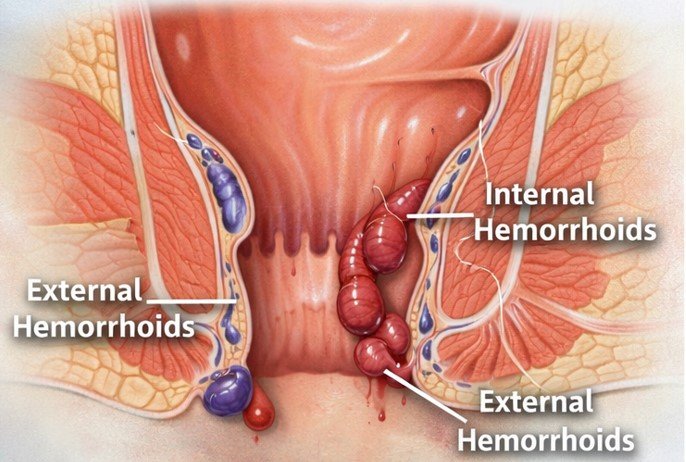
Understanding whether your hemorrhoids are internal or external helps explain your symptoms and guides treatment.
Internal Hemorrhoids
- Located inside the rectum, above the dentate line
- Covered by rectal mucosa (no pain receptors)
- Symptoms: Usually painless bleeding (bright red blood), possible prolapse (coming out of the anus), mucus discharge
- Treatment response: Respond well to rubber band ligation, sclerotherapy, infrared coagulation (for Grades I–II), and procedures like THD or laser (for Grades II–III)
External Hemorrhoids
- Located under the skin around the anus, below the dentate line
- Covered by skin (has pain receptors)
- Symptoms: Usually painless unless thrombosed (clotted), visible and palpable lumps, swelling, itching
- Treatment response: Conservative care for most; thrombosed ones may benefit from excision within 48–72 hours; large skin tags often removed surgically
Mixed Hemorrhoids
Many patients have both internal and external components. This is common in Grade III and IV hemorrhoids.
Hemorrhoid Grading System: Why It Changes Everything
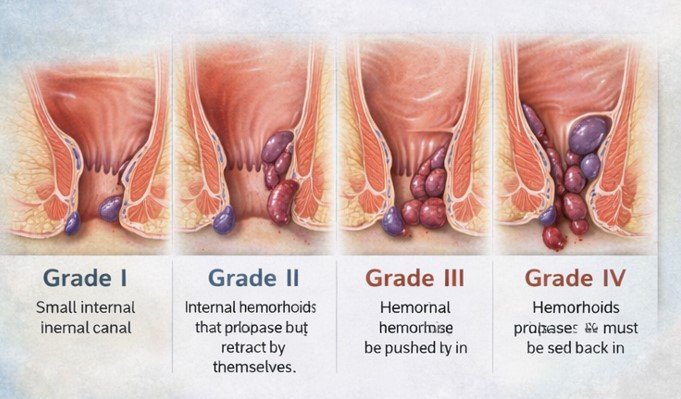
Grade I
- Hemorrhoids bleed but don't prolapse (don't come out)
- You can't see or feel them
- Typical treatment: Dietary changes, fiber, hydration, topical treatments; office procedures like rubber band ligation if bleeding persists
Grade II
- Hemorrhoids prolapse during straining or bowel movements but go back inside on their own
- You might feel them briefly but they disappear
- Typical treatment: Rubber band ligation, sclerotherapy, infrared coagulation; sometimes laser or THD for larger Grade II
Grade III
- Hemorrhoids prolapse and require manual reduction (you have to push them back in with your finger)
- They don't stay inside on their own after a bowel movement
- Typical treatment: THD/HAL-RAR, laser hemorrhoidoplasty, or hemorrhoidectomy (surgery), depending on size and anatomy
Grade IV
- Hemorrhoids are permanently prolapsed and cannot be pushed back inside
- They stay outside all the time
- Typical treatment: Usually hemorrhoidectomy (surgical removal); occasionally THD if there's minimal external component
Why grading matters: Different treatments work for different grades. It's important to understand that treatment should be matched to your specific anatomy and grade. A Grade IV hemorrhoid typically requires surgical excision, while a Grade I hemorrhoid often responds to conservative measures. The safest approach is grade-based treatment selection, not a one-size-fits-all technique.
What Causes Hemorrhoids? (And Dubai-Specific Risk Factors)
Hemorrhoids develop when there's increased pressure on the blood vessels in the rectum and anus. Common causes include:
Straining during bowel movements
Chronic constipation and hard stools are among the most common culprits. When you strain, you increase pressure in the abdomen and pelvis, which engorges hemorrhoidal vessels.
Prolonged sitting
Sitting for long periods—especially on the toilet—increases pressure on anal veins. In Dubai, I see this frequently in office workers who sit 10–12 hours a day in air-conditioned environments.
Chronic diarrhea
Repeated diarrhea irritates the anus and increases pressure.
Low-fiber diet
A diet low in fiber leads to hard stools and straining. Many expatriates in the UAE eat less fiber than they did in their home countries.
Dehydration
Dubai's heat and air conditioning can lead to dehydration, making stools harder. If you're not drinking enough water—especially in summer—you're at higher risk.
Pregnancy and childbirth
The growing uterus increases pressure on pelvic veins, and straining during delivery can cause or worsen hemorrhoids. Hormonal changes also relax vein walls.
Aging
The tissues supporting hemorrhoids weaken with age. Hemorrhoids are most common between ages 45 and 65.
Heavy lifting
Repeated heavy lifting (gym, manual labor) increases abdominal pressure.
Obesity
Extra weight increases pressure on pelvic veins.
Genetics
Hemorrhoids tend to run in families. If your parents had them, you're more likely to develop them.
Dubai lifestyle factors: In my Dubai practice, I see certain patterns: office workers with long sitting hours, dehydration from relying on coffee and tea rather than water, low fiber intake (eating out frequently, processed foods), and delayed medical care because of busy work schedules or embarrassment.
Treatment Options in Dubai: From Conservative Care to Surgery
Conservative Treatment (First-Line for All Grades)
Before considering any procedure, we start with lifestyle and dietary changes. For Grade I and early Grade II hemorrhoids, this is often all you need.
Dietary changes: fiber and hydration
- Goal: Softer, bulkier stools that pass easily without straining
- Fiber target: 25–35 grams daily (fruits, vegetables, whole grains, legumes)
- Hydration: 2.5–3 liters water daily in Dubai's climate (more if you exercise)
- Fiber supplements: Psyllium (Metamucil, Fybogel) or methylcellulose if diet alone isn't enough
Toilet habits
- Don't strain or hold your breath
- Don't sit on the toilet for more than 5 minutes (put your phone away)
- Go when you feel the urge; don't delay
- Consider a footstool to elevate knees (squatting position opens anorectal angle)
Topical treatments
- Over-the-counter creams or suppositories (hydrocortisone, witch hazel, lidocaine) provide temporary symptom relief
- Reduce swelling, itching, and discomfort, but don't cure hemorrhoids
- Use short-term (a few days to a week), not long-term
Sitz baths
- Sitting in warm water 10–15 minutes, 2–3 times daily, especially after bowel movements
- Soothes irritation and keeps the area clean
Office Procedures (for Grade I–II, Some Grade III)
These are done in-office, usually without general anesthesia. You go home the same day and return to normal activities quickly.
Rubber Band Ligation
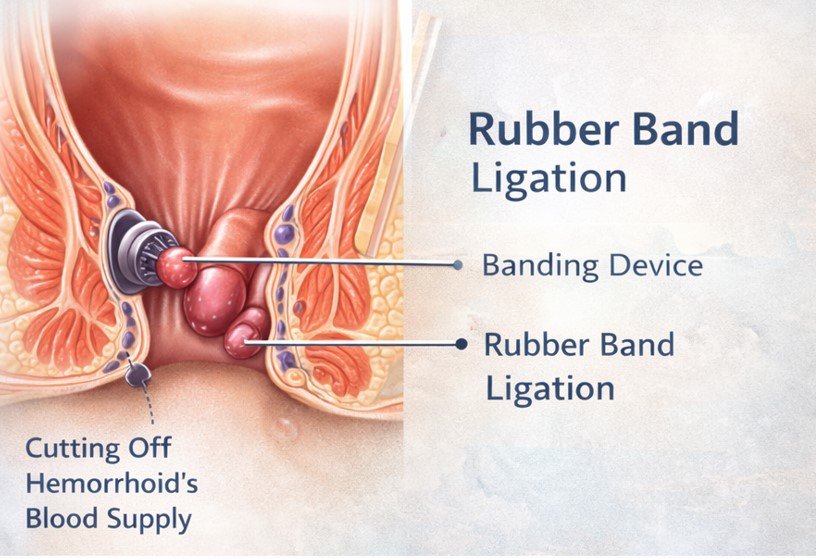
- Best for: Grade I & II, some small Grade III internal hemorrhoids
- Anesthesia: None (area has no pain receptors)
- Recovery: Minimal; mild pressure/discomfort for 1–2 days
- Success rate: High for appropriate grades; often 1–3 sessions
- Limitations: Large Grade III/IV, significant external component, low hemorrhoids
Sclerotherapy (Injection Treatment)
- Injection causes hemorrhoid to shrink and scar
- Best for: Grade I & small Grade II internal hemorrhoids
- Anesthesia: None; recovery immediate
- Less effective than banding for larger hemorrhoids
Infrared Coagulation
- Infrared light applied to base of hemorrhoid, creating scar tissue to cut blood supply
- Best for: Grade I & small Grade II
- Anesthesia: None; recovery immediate
- Success: Good for early grades; multiple sessions may be needed
Minimally Invasive Operating Room Procedures
For Grade II–III not responding to office procedures or select Grade IV cases.
Laser Hemorrhoidoplasty (LHP)
- Laser fiber shrinks hemorrhoid from inside
- Best for: Grade II & III internal hemorrhoids
- Anesthesia: Local with sedation or spinal
- Recovery: 3–7 days; mild-moderate discomfort, return to desk work in few days
- Limitations: Not for Grade IV or large external hemorrhoids; recurrence possible
THD / HAL-RAR
- Arteries supplying hemorrhoids are tied off; prolapsed tissue lifted/stiched back (mucopexy)
- Best for: Grade II & III, select Grade IV (without large external component)
- Anesthesia: Spinal or general
- Recovery: 5–10 days; less painful than hemorrhoidectomy
- Advantages: Preserves tissue, faster recovery
- Limitations: Not for large external hemorrhoids; specialized equipment required
Stapled Hemorrhoidopexy (PPH)
- Circular stapler removes rectal tissue, pulls hemorrhoids back up
- Best for: Select Grade III & IV internal hemorrhoids
- Anesthesia: General or spinal
- Recovery: 7–14 days; less pain than excisional hemorrhoidectomy
- Limitations: Higher recurrence than surgery; rare complications; not suitable with external component
Surgical Treatment: Hemorrhoidectomy
- For Grade IV, large mixed hemorrhoids, or failed less invasive treatments
- Techniques: Open (Milligan-Morgan), Closed (Ferguson), Laser/Diathermy-assisted
- Anesthesia: General or spinal; hospital stay day-case or overnight
- Recovery: 2–4 weeks most activities, full healing 6–8 weeks
- Success rate: Highest; low recurrence
- Pain: Managed with medication; first week most uncomfortable
When surgery is necessary: Grade IV, large external components, or severe symptoms despite other treatments. Surgery provides the most reliable long-term cure.
My Approach: What Sets This Practice Apart
In my years of practice across multiple countries and continents, I've learned that hemorrhoid treatment isn't just about technical skill—it's about listening to patients and matching the treatment to their specific situation, not to what equipment happens to be in the clinic.
If you were my brother or sister dealing with hemorrhoid symptoms, here's what I'd tell you:
- Don't be embarrassed—I see this every day, and your symptoms aren't unusual or shocking.
- Make sure you get a proper examination before agreeing to any treatment.
- Different treatments work for different grades. The safest approach is matching treatment to your specific anatomy.
In Dubai specifically, I see patterns related to lifestyle: long hours at a desk, air conditioning leading to dehydration, eating out frequently (lower fiber), and international travel disrupting bowel habits. These factors matter, and addressing them is part of every treatment plan I create.
What I look for during examination is not just the hemorrhoids themselves, but the whole picture: Are there skin tags suggesting previous thrombosed hemorrhoids? Is there evidence of chronic straining (anal fissure, tight sphincter)? Are the hemorrhoids truly Grade III, or are they early Grade IV that won't respond to banding? These details change the treatment approach, and you can't get them from symptoms alone.
Frequently Asked Questions
No. While hemorrhoids are a common cause of bright red rectal bleeding, other conditions can also cause bleeding — fissures, fistulas, polyps, inflammatory bowel disease, and colorectal cancer.
If you're bleeding, you need an examination to confirm the cause, especially if you're over 40, have family history of colon cancer, or symptoms like weight loss or bowel habit changes.
If you're under 40 with no red flags and hemorrhoids clearly explain symptoms, colonoscopy may not be needed immediately.
If you're 40+ and haven't had screening, colonoscopy is recommended even if hemorrhoids are present — both conditions can coexist.
In the UAE, screening typically begins at age 40.
Grade I may resolve with diet, fiber, and hydration.
Grade II may improve but often needs rubber band ligation.
Grade III and IV usually require intervention like THD, laser, or surgery.
- Grade I–II: Banding, sclerotherapy, infrared coagulation
- Grade II–III: Laser or THD
- Grade IV / mixed: Hemorrhoidectomy
The safest approach is matching treatment to your specific anatomy.
Laser is less painful than traditional surgery but not painless. Expect discomfort for several days.
“Scar-free” is misleading — all procedures create healing response. Marketing often overpromises.
A thrombosed external hemorrhoid is a clot causing a painful lump.
Pain peaks in 48–72 hours. Early removal provides relief; later it often improves naturally.
First week is uncomfortable with moderate to severe pain, especially during bowel movements.
Improves by week two. Full recovery usually 4–6 weeks.
No. Hemorrhoids are not cancer and don't turn into cancer.
However, symptoms can overlap — proper examination is important.
Yes. Increased pressure and hormonal changes contribute.
Most improve after delivery. Surgery usually postponed until after breastfeeding.
- Fruits (berries, pears, apples)
- Vegetables (broccoli, carrots, leafy greens)
- Whole grains (oats, brown rice)
- Legumes (lentils, beans)
Drink 2.5–3 liters of water daily. Avoid low-fiber processed foods.
Yes. Prolonged sitting increases pressure on anal veins.
Take breaks hourly and avoid sitting on toilet more than 5 minutes.
Yes. Walking, swimming, yoga are helpful.
Avoid heavy lifting until symptoms improve.
- Banding: 1–2 days
- Laser/THD: 3–7 days (desk), 7–14 (physical)
- Hemorrhoidectomy: 7–14 (desk), 14–21 (manual)
Recurrence depends on treatment and bowel habits.
Hemorrhoidectomy has lowest recurrence rate.
A small lighted scope is inserted briefly to visualize internal hemorrhoids.
Takes 1–2 minutes and causes mild pressure only.
- Office procedures: No fasting
- Sedation/surgery: Fast 6–8 hours
Yes. Stay hydrated and bring stool softeners if recently treated.
Most UAE plans cover medically necessary treatment.
Elective procedures vary by policy.
Yes. All consultations and treatments are fully confidential.
- Colorectal fellowship training
- Board certification
- Experience with all treatments
- Proper examination
- Honest discussion of options
References and Medical Sources
- UAE Colorectal Cancer Screening Guidelines – Abu Dhabi Department of Health recommends screening starting at age 40 for average-risk individuals. Abu Dhabi Public Health Center – Colorectal Cancer Program
- Cleveland Clinic Abu Dhabi – Local clinical protocols for UAE population. CCAD Screening Guidelines
- Thrombosed External Hemorrhoids Treatment – Evidence for 48–72 hour intervention window. Greenspon J, Williams SB, Young HA, Orkin BA. Thrombosed external hemorrhoids: outcome after conservative or surgical management. Dis Colon Rectum. 2004;47(9):1493-8. PubMed
- Transanal Hemorrhoidal Dearterialization (THD) Outcomes – Success rates for Grade II–III hemorrhoids. Ratto C, Giordano P, Donisi L, et al. Transanal haemorrhoidal dearterialisation (THD) for haemorrhoidal disease: a single-centre study on 1000 consecutive cases. Colorectal Dis. 2017;19(8):750-756. PubMed
- American Society of Colon and Rectal Surgeons Clinical Practice Guidelines – Evidence-based hemorrhoid treatment recommendations. Davis BR, Lee-Kong SA, Migaly J, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum. 2018;61(3):284-292. PubMed
- Rubber Band Ligation Effectiveness – Long-term outcomes for hemorrhoid banding. Shanmugam V, Thaha MA, Rabindranath KS, Campbell KL, Steele RJ, Loudon MA. Rubber band ligation versus excisional haemorrhoidectomy for haemorrhoids. Cochrane Database Syst Rev. 2005;(3):CD005034. PubMed
Medical Review: This content was written and reviewed by Professor Dr. Antonio Privitera, Consultant Colorectal Surgeon, with fellowship training at the Mayo Clinic and Royal College of Surgeons (UK), and European Board Certification in Colorectal Surgery.
Locations and Booking
I see patients at multiple locations across Dubai and Abu Dhabi. For specific clinic addresses and to confirm current availability at each location, please contact us directly.
Schedule a Discreet Consultation
If you're experiencing hemorrhoid symptoms — bleeding, discomfort, prolapse, or itching — I'm here to help. The first step is an accurate diagnosis, and together we'll develop a treatment plan tailored to your grade and lifestyle.
Same-day and next-day appointments are often available. All consultations are private and confidential.
Professor Dr. Antonio Privitera
Consultant Colorectal Surgeon
Fellowship Training: Mayo Clinic | Royal College of Surgeons (UK)
European Board Certified in Colorectal Surgery
About the Author

Dr. Privitera is the only surgeon in the world with both a Mayo Clinic (Rochester, USA) and University of London Colorectal Surgery Fellowship. He completed an advanced laparoscopic and robotic fellowship in Seoul, South Korea.
He previously served as Lead Colorectal Surgeon at Tawam Hospital–Johns Hopkins Abu Dhabi and Associate Professor at UAE University.
He is a Fellow of the American Society of Colon and Rectal Surgery (FASCRS), Fellow of the Royal College of Surgeons of England (FRCS), and author of over 70 peer-reviewed publications. He also served as General Secretary of the Emirates Society of Colon and Rectal Surgery (2021–2024).
He practices across Dubai and Abu Dhabi.
