Anal Fistula
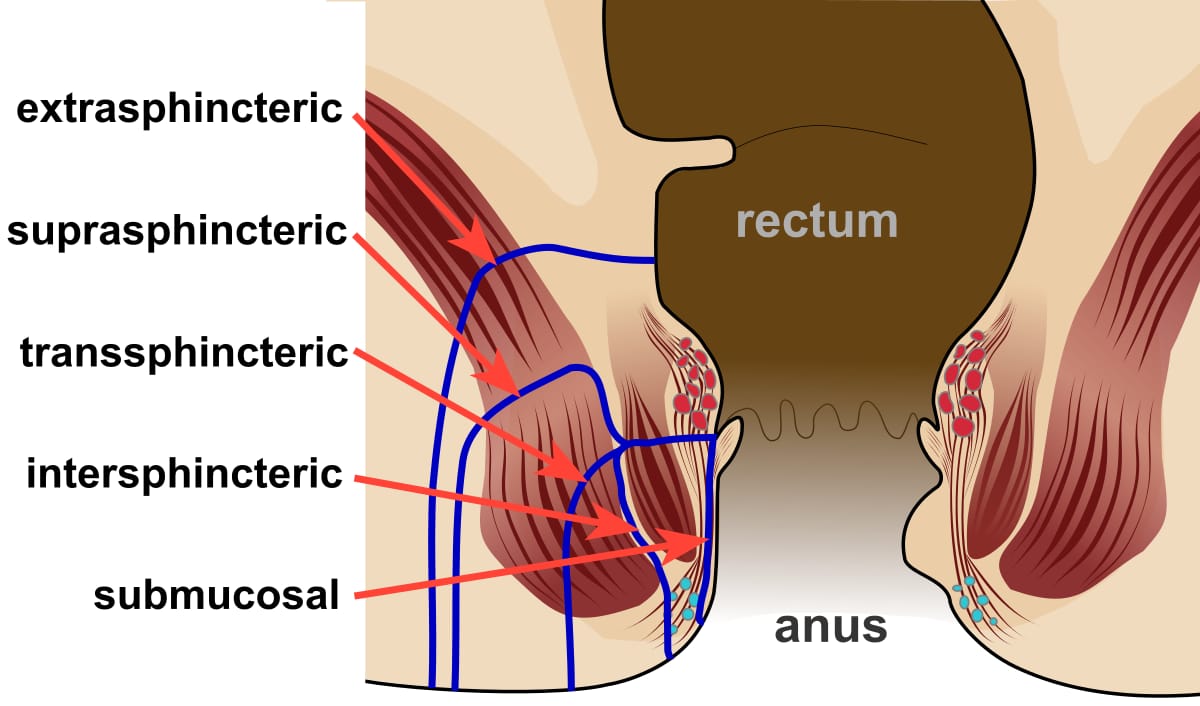
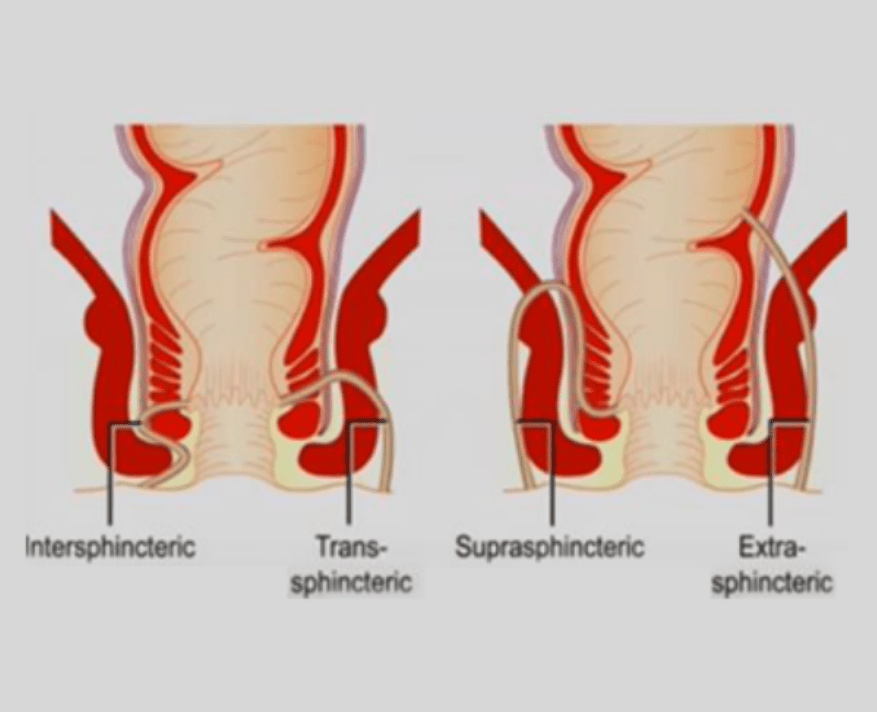
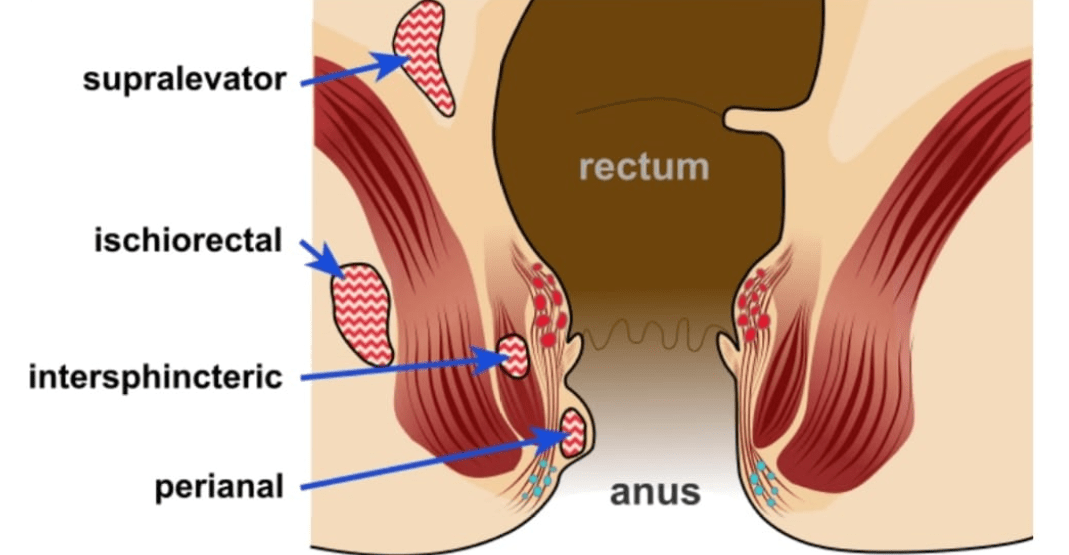
An anal fistula is a persistent communication or tract, covered by epithelium, between the inside of the anal canal and the perianal skin. Anal fistula can be submucosal, inter-sphincteric, trans-sphincteric, suprasphincteric, or extrasphincteric. They may have a single tract or multiple tracts and secondary branches. Low transsphincteric fistulas involving less than 1/3 of the muscles and intersphincteric fistulas are considered simple fistulae. Complex fistulas are transsphincteric with > 1/3 muscle involvement, extrasphincteric, or suprasphincteric. Most fistulas are cryptoglandular in origin and caused by infection of the anal glands situated in the intersphincteric space with their duct opening at the level of the dentate line. Other causes of fistula formation include Crohn’s disease, radiation, trauma, malignancy, infectious diseases, etc.
Symptoms of Anal Fistula
Patients usually present with anal pain, perianal pain, discharge (sero-sanguineous or purulent), fever, perianal induration, or a fluctuant abscess. It is important that are diseases are considered in the differential diagnosis: hidradenitis suppurativa, furuncles, pilonidal disease, etc.
Diagnosis of Anal Fistula
According to Goodsall’s law, external orifices that are situated posteriorly to a line drawn transversely in the mid part of the anus will have their internal opening at 6 o’clock. External orifices anterior to this line will have the corresponding internal orifice at the same level as the fistula tract runs in a radial direction.
Anal Fistula Treatment
Most surgeons carry out anal fistula treatment. However, patients must be aware that the best results of anal fistula treatment are achieved by colorectal surgeons that have a thorough understanding of the disease and that are skilled with the vast array of minimally invasive techniques. This allows treatment to be tailored to each patient to successfully heal the fistula with no risk of incontinence. Fecal incontinence is a severe long-lasting complication of improper anal fistula surgery and severely impairs the quality of life. The best anal fistula treatment is offered by fellowship-trained colorectal surgeons with a long history of committed practice in the field.
Methods of Anal Fistula Surgery
Anal fistula surgery encompasses a wide variety of techniques ranging from traditional fistulotomy, fistulectomy, loose seton, cutting seton to minimally invasive techniques including : Ligation of the Inter-sphincteric Fistula Tract (LIFT), Video-Assisted Anal Fistula Treatment (VAAFT), Fistula Laser Closure (FiLAC), endoanal and endorectal advancement flap, fibrin glue, bioprosthetic plugs and stem cell treatment.
The best anal fistula surgery would resolve the infection and achieve healing of the tract while preserving the integrity of the anal sphincters, thus avoiding fecal incontinence. In the case of simple fistulas involving only the distal part of the sphincters, traditional lay-open of the tract (fistulotomy) or complete excision (fistulectomy) can achieve healing rates up to 100% with low risk of incontinence (< 10%). In patients with already impaired continence for other reasons (e.g. obstetric traumas), or at risk having had previous irradiation or suffering from Crohn’s disease, a worsening in their function may be expected. In cases where the involvement of the sphincters is > 30 %, the anal incontinence risk is high and other techniques for anal fistula treatment should be considered.
Minimally Invasive Anal Fistula Surgery
Minimally invasive techniques of anal fistula surgery have flourished in the last few years to eliminate the risk of incontinence by completely preserving the sphincter complex. The success rate of these techniques is about 70%. In case of failure, these techniques can be repeated or more invasive procedures may be considered.
Stem Cell Treatment for Anal Fistula
The use of Adipose-derived stem cells (ASCs) is an appealing approach in anal fistula surgery as mesenchymal cells can differentiate into other types of cells and promote healing. The number of stem cells obtained from the subcutaneous tissue by liposuction is one hundred times higher than bone marrow aspirates. The fistula tract is debrided and the internal orifice closed with sutures. ASCs are injected in and around the fistula tract and fibrin glue used for sealing. The initial enthusiasm with this technique faded when results showed low success rates over a longer period.
Fistula Laser Closure (FiLaC)
The laser treatment for anal fistula was first reported in 2011. The advantage of this technique is to destroy the epithelium lining the anal fistula tract and at the same time obliterate its lumen. This is obtained by the energy delivered homogeneously at 360 degrees by a laser probe that is withdrawn 1 cm every 3 sec until the whole tract is sealed. Conversely, the use of simple cautery is not able to completely remove the epithelium and the persistence of this is one of the main factors preventing fistula closure. Also, shrinkage of the tract is a unique advantage of the laser. Most surgeons will also close the internal orifice with an endorectal flap or with a figure-of-eight suture. Success rates up to 80% have been reported.
Seton Placement for Anal Fistula
This is the oldest technique of anal fistula surgery initially described by Hippocrates and based on the insertion of foreign material in the fistula tract (Silk, rubber threads, etc.) that is either left untied (loose seton) or tied (cutting seton). A loose seton will prevent infection and recurrence of the abscess and will allow for a healing process that will facilitate a second stage procedure. A cutting seton is based on the assumption that allowing for a gradual severing of the sphincters and formation of scar tissue, the two cut ends of the muscle would stay attached. The recurrence rate of anal fistula surgery with a cutting seton ranges from 22% to 39%. More recently, some modifications of the cutting seton technique have reported a very low recurrence rate and no serious cases of incontinence.
Anal Fistula Plug
The anal fistula plug is derived for porcine intestinal submucosa and it is inserted in the anal fistula tract to promote tissue healing. It is also a material very resistant to infections. The absence of infection and gentle debridement and cleaning of the tract is pivotal for the success of this type of anal fistula surgery. One of the most common reasons for failure is related to the extrusion of the plug possibly for a non-optimal fixation of the material in situ. Therefore, other materials have been introduced, such as GORE BioA® plug. However, because of the low and variable success rate (average 50%) and the high cost of the procedure, the plug technique has been abandoned by most surgeons.
VAAFT – Video Assisted Anal Fistula Treatment
The VAAFT technique was first introduced in Italy in 2006. A fistuloscope is inserted through the external opening and allows to visualize the main tract and any secondary branches. A diathermy probe can be inserted to cauterize the wall of the fistula. At the same time, continuous irrigation with a solution of glycine-mannitol 1% keeps the tract open, washes out any debris, and represents a good energy conductor. A brush is also part of the kit and allows the removal of granulation tissue and debris. The internal fistulous orifice is closed with a flap or with the use of a stapling device. Success rates over 70% have been reported.
Fibrin Glue for the treatment of Anal Fistula
The initial results of fibrin glue injection into the fistula tract were promising. Stimulation of fibroblasts and pluripotent cells were meant to result in the closure of the anal fistula. However, a high recurrence rate was noted especially on longer follow-up. The liquid consistency of the glue may be one of the causes of the inability to fill the tract. Also, the possibility of infection and formation of a secondary tract has been reported in up to 3% of cases. Better results have been shown in tracts > 4 cm, possibly for a better chance to hold the material. Most surgeons have abandoned fibrin glue as a single treatment for anal fistula. Nonetheless, fibrin glue may be an adjunct to other techniques, such as VAAFT, for its inherent ability to promote healing.
LIFT Procedure for Anal Fistula
The Ligation of the Intersphincteric Fistula Tract (LIFT), was first described by Rojanasakul in 2006. The technique involves an incision in the intersphincteric groove and dissection through the intersphincteric space until the fistula tract is encountered. Insertion of a soft catheter (ureteric catheter – personal preference) into the fistula allows for easy identification of the tract that is dissected, divided, and ligated at this level with absorbable sutures. The subcutaneous part of the tract is curetted and will slowly heal as the connection with the anal canal is interrupted. The wound is closed with absorbable material. A Metanalysis (2015) of 24 studies concluded that the LIFT procedures achieve up to 76% healing rate with 0% incontinence rate and 5.5% of complications. A higher risk of recurrence has been found in patients with previous fistula operations, likely because of the scar tissue and inability to properly identify the fistula tract. Better results have been noticed in patients having a loose seton placed before the procedure, showing that the absence of infection is paramount to obtain the best results. Modifications of the technique with the insertion of a bioprosthetic graft in the intersphincteric space as a barrier between the two cut ends of the fistula tract have been described.
Emergency Surgery for Anal Fistula
An Anal fistula may present with an anorectal abscess that may require surgical drainage. The incision must be made close to the anal verge to minimize the length of the tract in case of fistula formation. The concomitant presence of an anal fistula (30-70%) can be treated with the insertion of a loose Seton to prevent recurrence of the abscess. However, in consideration of the fact that 50% of the anal fistulas in this setting heal spontaneously, placement of a seton may be avoided with the understanding of a higher risk of recurrence of abscess. A very low anal fistula can be laid open, but the general rule is not to perform a fistulotomy in case of an abscess as the surgical field is infected and the degree of involvement of the anal sphincters may not be accurately evaluated due to tissue edema. Incision and drainage are usually sufficient and antibiotics are given in case of systemic signs of infection or gross cellulitis.
FAQs About Anal Fistula
No. Anal fistulas do not heal on their own and almost always require surgical treatment.
When performed by an experienced colorectal surgeon using sphincter-preserving techniques, fistula surgery is safe with low complication rates.
Dr. Antonio prioritizes techniques that protect the anal sphincter, minimizing the risk of incontinence.
Most patients return to normal activities within days to two weeks depending on the procedure.
Most fistulas develop after an anal abscess. Crohn’s disease and previous anorectal surgery are other causes.
Results after Anal Fistula Surgery
The overall healing rate of the anal fistula with the new minimally invasive techniques that allow for sphincter preservation is around 70%. This means that 3 out of 10 will fail treatment and will need either a second attempt with the same or other sphincter-preserving procedures or will have to undergo more traditional treatments. The LIFT procedure represents a good compromise between new and old techniques with an overall high success rate. When the fistula is intersphincteric or low transsphincteric involving <1/3 of the external sphincter muscle, a minor possibility of incontinence may well be accepted given the high healing rates approaching 100%. If a patient has previously impaired continence, then minimally invasive techniques become a priority because minimal division of the anal muscles may well worsen symptoms. It is mandatory to have a full and honest discussion with the patient explaining the pros and cons of each procedure and come up with a tailored treatment plan that will lead to the best results without affecting the quality of life.
Looking for an Anal Fistula Doctor in Dubai and Abu Dhabi?
A proctology service not only for Anal Fistula Surgery in Dubai and Abu Dhabi but also for many other diseases is currently operating in Dubai London Hospital, Aster Hospital, American Hospital. Currently, Dr. Antonio Privitera is offering a free consultation for anal fistula treatment in the same hospital in Dubai and Abu Dhabi.
