Anal Fissure Treatment
What is an Anal Fissure?
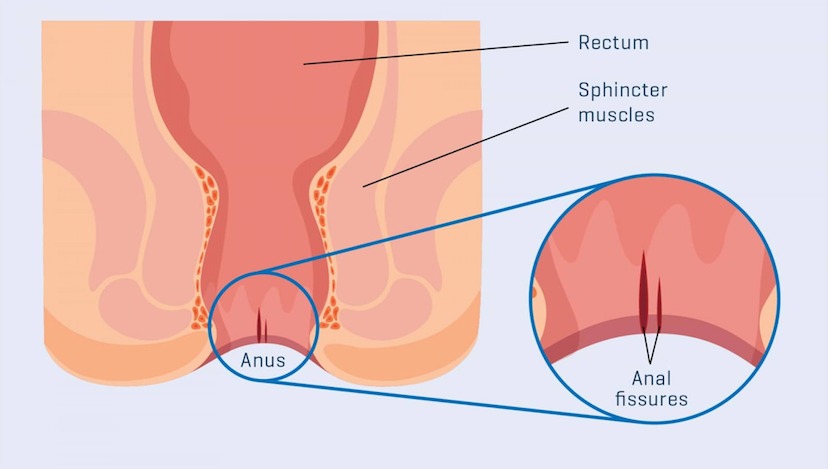
An Anal fissure is a tear in the mucosa and submucosa of the anal canal below the dentate line. It can be acute or chronic if persists for > 6 weeks. Anal fissures are associated with pain and bleeding during bowel movements. Anal fissures are often seen in patients with chronic constipation or diarrhea. They are also common in women after childbirth.
What are the Causes of Anal Fissure?
Although the mechanism of anal fissure formation is not completely understood, an imbalance between rectal and anal pressures is a key factor. Passage of hard stool, straining during defecation, and the inability of the anal sphincter to fully relax will lead to a traumatic tear of the anoderm. Studies have shown an increased anal tone in patients with an anal fissure, but it is not clear whether this is a consequence of the fissure or a pre-existing factor. Most anal fissures (90%) are posterior and only 10% are anterior. Anterior anal fissures are more common in females. It is postulated that during defecation, the pressure is mostly exerted on the posterior side of the anal canal. Also, cadaveric studies have shown a decreased blood supply of the anal mucosa posteriorly suggesting a mechanism of ischemia as a contributing factor. Most anal fissures occur anteriorly or posteriorly in the midline. Only 1% of fissures are located in other positions and they are referred to as ‘atypical’. Differential diagnosis includes Crohn’s disease, tuberculosis, syphilis, anal cancer, herpes, etc. As regards Crohn’s disease, the occurrence of fissures is not unusual especially in the setting of proctitis. Treatment should focus on the primary disease with biologics and immunosuppressants before contemplating surgical options.
Anal Fissure Symptoms
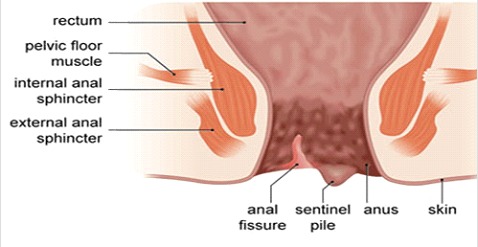
Pain is present in more than 90% of patients and typically occurs during defecation and lasts from a few minutes to several hours and is severe and sharp. Bleeding is reported > 70% of cases and is either seen on the toilet paper or dropping on top of the stool. The diagnosis is usually straightforward, however, anal fissures may not be immediately visible because of sphincter spasm. In these cases, asking the patient to push simulating a bowel movement, and gently parting the buttocks, may reveal the fissure. Applying local anesthetic gel and waiting for a few minutes may make the examination more comfortable and accurate. A sentinel tag and a hypertrophied papilla may be seen in chronic anal fissure. Usually, finger rectal examination and anoscopy are avoided in the acute setting because of pain. Nevertheless, these need to be carried out once symptoms settle to rule out other conditions.
01. Siz Baths
02. Tropical Nitrates and Calcium Antagonist Medications
03. Fiber Supplements
04. Botulinum Toxin
Anal Fissure Treatment
Most anal fissures will heal with conservative measures without the need for surgical treatment. Chronic fissures are less prone to heal. Avoiding and treating constipation, straining and other causes of anal trauma are the mainstay of anal fissure treatment. Dietary changes (high fiber diet and increased water intake) are advised and stool softeners are prescribed. Anal muscle relaxant ointments or botulinum toxin injection are other important components of anal fissure nonsurgical treatment.
Siz Baths
Warm Sitz baths are recommended in anal fissure treatment to reduce pain and anal spasm. Manometric studies have shown that immersion at a temperature of 40°C for 5 minutes, significantly decrease anal pressures.
Topical Nitrates and Calcium Antagonist Medications
Glyceryl trinitrate (GTN) ointment is significantly better than a placebo in anal fissure treatment. The most commonly used dose is 0.2% that is applied over the anal verge two times a day for 8 weeks. The main side effect of this medication is a headache due to systemic absorption and vasodilatation. Up to 20% of patients need to discontinue the medication for this reason. Anal applications of Nifedipine 0.5% or diltiazem 2% ointment three times daily is highly effective. Itching is the main side effect of this class of medications but is less likely to cause discontinuation of treatment.
Fiber Supplements
Fiber supplements are highly effective in anal fissure treatment. A randomized controlled trial showed that 10 g of bran fiber two times a day and warm sitz baths after bowel movements resulted in better control of pain and faster healing at 3 weeks compared with 2% lidocaine or 2% hydrocortisone cream. Another study reported that 15 g of bran daily in 3 divided doses was associated with fewer recurrences compared with a lower intake of 7.5 g.
Botulinum Toxin
Botulinum toxin injection was first reported in 1933 as a new anal fissure treatment. Botulinum toxin is significantly more effective than a placebo and can be used in combination with topical muscle relaxant medications. The dose and site of injection have been a source of debate. Most reputable centers would inject at least 20 U of the toxin on both sides of the anal canal (40 U) or a total of 40 U at each of the four quadrants. Botulinum toxin has usually a diffusion area of 1 cm, therefore it does not seem to matter whether it is injected directly into the internal anal sphincter or in the intersphincteric space. Systemic side effects are extremely uncommon but temporary flatus incontinence is observed in 18% of cases and stool incontinence in 5%. Perianal hematomas and perianal thrombosis have been reported following injection.
Anal Fissure treatment
Anal fissure surgery should be the last resort as most of the time proper conservative treatment is effective. Many procedures have been described in anal fissure surgery including anal dilatation, lateral internal sphincterotomy, advancement flaps, and fissurectomy.
Anal Dilation
Anal dilatation was the first anal fissure surgery reported in the literature. However, anal dilatation has been abandoned in favor of lateral internal sphincterotomy. A Cochrane Review showed that lateral internal sphincterotomy was associated with a significantly lower risk of flatus and fecal incontinence when compared with anal stretch. Also, the healing rate of the anal fissure was significantly higher.
Lateral Internal Sphincterotomy
The partial division of the internal sphincter is a highly effective anal fissure treatment with the downside of anal incontinence. Originally, a sphincterotomy was performed in the midline posteriorly and this was associated with a high rate of flatus impairment in 34% of cases and incontinence rate in 15%. This technique resulted in large posterior wounds with abnormal healing leading to a “key-hole deformity.” Nowadays, lateral internal sphincterotomy is performed either at 3 or 9 ‘o’clock. As regards the length of muscles to be divided, this has been the focus of extensive debate. Currently, colorectal surgeons would divide the muscle only up to the upper level of the anal fissure. With this tailored approach results have been very encouraging with 99% initial healing rate, <1% urgency, 1% incontinence of gas, and 35% of minor soling. No reports of incontinence to solid or liquid stool have been reported.
An expert surgeon (colorectal surgeon) must perform this procedure to limit the amount of muscle divided and to make sure that the muscle is actually divided. A study showed that 70% of patients with persistent fissures after sphincterotomy had no ultrasound evidence of internal sphincter division. Excision of hypertrophied anal papillae during lateral internal sphincterotomy has been shown to improve healing rates.
Advancement Flaps
Advancement flaps have been used successfully in anal fissure surgery for the treatment of nonhealing fissures. The flap usually consists of a skin and subcutaneous flap that is developed distally to the fissure. Minimal cautery should be used to avoid injury to the internal sphincter. The flap should be at least 1.5 times the length of the fissure and the base at least twice its width. High healing rates have been observed with this surgical approach. Complications include infection, bleeding, and dehiscence of the flap.
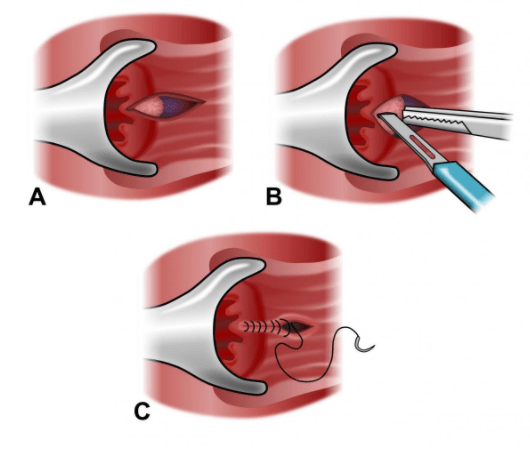
Fissurectomy
Fissurectomy involves the excision of the anal fissure margins, curettage of the base with the removal of granulation tissue, and excision of any hypertrophied papilla or scar tissue. The wound is either sutured or left open. One clinical trial showed that the results of fissurectomy were inferior to those of lateral internal sphincterotomy. Another study investigating the combination of fissurectomy with botulinum toxin reported a 93% healing rate and temporary flatus incontinence in 7% of cases.
FAQs About Anal Fissure
Acute fissures may heal with conservative treatment. Chronic fissures lasting more than 6-8 weeks usually require medical or surgical intervention.
Most patients experience significant pain relief shortly after surgery with minimal postoperative discomfort.
Treatment depends on severity. Options include topical medications, sitz baths, dietary changes, and lateral internal sphincterotomy for chronic cases.
When performed correctly, lateral internal sphincterotomy has a very low risk of continence disturbance.
Most patients experience rapid improvement within days of starting treatment, with full healing in weeks.
Anal Fissure Treatment - Recovery
Anal fissures are very commonly encountered in the daily practice of a colorectal surgeon. Conservative management is to be tried first and this is usually successful in > 90% of cases. Treating constipation and straining with changes in the diet and addition of bulking agents is paramount. The associated increased anal tone is addressed with the use of topical muscle relaxant medications (GTN, calcium channel blockers, botulinum toxin). Topical anesthetic creams may reduce pain and consequently spasm. In the case of failed conservative treatment, anal fistula surgery with fissurectomy or advancement flap may be considered avoiding the risk of incontinence. This is particularly important in patients with low-pressure sphincters. Alternatively, lateral internal sphincterotomy tailored to the length of the fissure is highly effective with a low rate of minor incontinence that is usually transient.
Looking for An Anal Fissure Treatment in Dubai & Abu Dhabi?
A proctology service in Dubai and Abu Dhabi not only for Anal Fissure Treatment, but also for many other diseases is currently operating in Dubai London Hospital, Aster Hospital, American Hospital. Currently, Dr. Antonio Privitera is offering a free consultation for nonhealing anal fissure in the same hospital in Dubai and Abu Dhabi.
